Anti-Mullerian Hormone (AMH) is a substance produced by granulosa cells in ovarian follicles. It is produced by primary follicles and is highest in follicles that are in the preantral and small antral stage (less than 4mm in diameter). Because AMH is produced only in small follicles, it is believed to be a measure of the remaining egg supply.
Finding out your AMH level is low (0.5 – 1.0 ng/ml) is devastating for most women. It is believed that you can do nothing to improve your AMH levels. It is used, along with other hormone levels, to determine if you are an IVF candidate. Finding out that your AMH level is low or very low (less than .5 ng/ml) is hope crushing. You feel like the window on your fertility is closing or that it may have already closed.
I have been on TTCAL long enough to see many of our ladies who have low and very low AMH go on to PgAL and PAL. Some of these ladies conceived via IVF, some with donor eggs, some with their own, and some naturally. I asked our grads to share their stories to help remind our ladies with low AMH that it is just one test and it does not mean that you cannot get pregnant with a healthy pregnancy. Thank you to all of our graduates who replied with their stories and agreed to share them with you.
I would like to give special thanks to MsAmandaPants who provided me with a copy of her well thought out and researched reply that she gives to ladies who post about receiving low AMH results. I have included it in its entirety.
A special note on supplements: many of our grads used supplements while they were still TTC and credit those with helping them conceive. If you would like to take any of these supplements, please talk with your doctor first.
buggirl72, AMH .17
From MsAmandaPants – AMH is an indicator of ovarian reserve–how many eggs you have left. Low AMH itself won’t cause a miscarriage, but it might (but not necessarily) point to egg issues that could have contributed to it. Most research suggests that AMH has more to do with the quantity of your remaining eggs. There are different opinions on whether it is also an indicator of quality. While it does not necessarily indicate poor quality eggs, there are some that think that the eggs that remain at the end of your reserve may not be the highest quality, that higher quality eggs are selectively ovulated first, but there are differing opinions. AMH is also used as a predictor of how well you might respond to fertility drugs; low AMH is often correlated to poor response (but not necessarily so– I have shitty AMH and had a decent response).
It is important to keep in mind that AMH is only one marker of ovarian reserve and should always be considered in the context of your entire medical history, appropriate CD 3 blood work (estradiol, LH, FSH), and an antral follicle count. These are all critical parts of a whole that make up your entire fertility outlook.
Age naturally plays a role in decreasing AMH since egg reserves decrease with age; older women would be expected to have a naturally lower AMH range. While a lower normal range would be expected in AMA women, there is a threshold at which your AMH might be deemed irregularly low for your age. AMA + abnormally low AMH is a bit more worrisome because you are naturally dealing with older eggs and the quality issues that come with that, as well as a decreased reserve of quantity. There are some studies that show that low AMH in younger women is less of an issue because they typically have younger, higher quality eggs, in which case it is likely merely an issue of quantity/remaining eggs.
Other factors can artificially influence AMH readings and, again, it is important to understand it in context of our your entire fertility picture. This also means understanding factors that can influence and skew CD 3 blood work. For example, high estradiol can falsely suppress FSH. High FSH, particularly when combined with a low AMH could be indicative of diminished ovarian reserve. Low vitamin D can also artificially suppress AMH. Anyone that gets a low AMH reading, particularly if not AMA, should have their vitamin D checked to determine if it could be falsely lowering your score. Finally, from what I have read, the AMH test itself is fairly difficult to run/process and can be prone to errors. If you get a low initial AMH reading and don’t show any risk factors or corroborating blood work/antral follicle count, etc., I would encourage a recheck before resigning yourself to a dx of low or diminished ovarian reserve.
There are a lot of conflicting reports about whether you can improve your AMH through supplementation. DHEA, CoQ10 (or, even better, ubiquinol the more readily available for absorption version of CoQ10) to support your egg health, have been linked to possibly improved AMH readings. This is fairly controversial and without significant acceptance in the larger medical community. Talk to your doctor about whether supplementations might be helpful in your specific case. Do not start any supplements without consulting with your RE. There are significant drug interactions and supplementation can also do more harm than good. DHEA, in particular, is a hormone that can have negative consequences if taken without appropriate need and monitoring.
Take heart, whether AMA or not, a low AMH does not necessarily mean that you are going to run out of eggs next month. It may, however, mean that your window to conceive is shorter than the average person and that you may need to consider more aggressive treatment under the direction of your RE. Low AMH does NOT, repeat NOT, mean that you can not get pregnant and stay pregnant.
- MsAmandaPants – February 2012: 1st pregnancy: natural BFP after one month of trying. Ended in MMC and D&C.
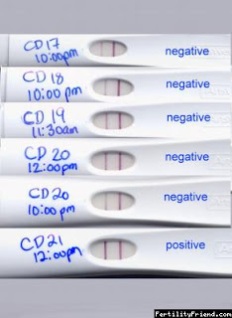
• April-October 2012: trying on our own with no success, despite temping, OPKs confirming ovulation, good timing, etc.
• November 2012: 2nd pregnancy: natural BFP after 6 or 7 cycles of trying with no luck, ultimately determined to be complete molar pregnancy
• December 2012: RPL/AMA testing, including AMH. AMH comes back at .53. Crushing. Diagnosed with low AMH, DOR, and complete molar pregnancy. Benched until August for molar pregnancy.
• August 2013: Recheck of AMH to determine how much it had decreased during mandatory bench time. It came back at .29. Devastating.
• August-October 2013: Started fertility treatments in August because of worsening AMH. 3 IUIs using Femara and injects (Menopur) and Ovidrel trigger. All failed, although I had a decent response to fertility drugs, 3, 4, 6 mature follicles, respectively).
• December 2013: We were told we would have to move to IVF. Recheck of AMH to see if ubiquinol was helping and to determine how much worse it had gotten before moving to IVF. It came back at .54, showing some improvement.
• A few days later in December 2013: Learned I was pregnant. I had been told that I had to move to IVF and was letting my body and brain rest from treatments for a couple of months before jumping into that. I got pregnant on my own, on a treatment break.
During my molar pregnancy mandatory bench time, I was exercising very heavily (training for half marathons) and I was also regularly taking between 200 and 300 of ubiquinol (the more bio-available version of coQ10) daily. I can’t say for certain that it was the result of my efforts, but my AMH did show improvement during this time. I also took high quality prenatals throughout the period I was TTC.
Grateful&Thankful AMH was .23 & my first RE told me there was no way to increase it. I took 2tsp daily of Royal Jelly & 300 mg of CoQ10 2x a day for 3 months. After retesting my AMH was .77
I don’t have any tubes so IVF was my only option any way. I got pregnant via IVF after taking those supplements for about 2.5 months. I miscarried due to a SCH. I’m currently pregnant again after IVF 5.5
I wanted to add that I’ve heard RJ can make fibroids grow so if you have trouble with fibroids, you may want to tone down your dosage.
2MomsinCA – Hi! Low AMH was devastating. I did a full work up with the RE before even attempting to ttc so I found out I had an AMH of .8 early on. My paperwork at every RE appt from then on said my diagnosis was “diminished ovarian reserve.” Ouch.
I took ubiquinol coq10, L-arginine, and pure royal jelly daily for about 4 months during the ttc process. I also practiced yoga and abdominal massage through the whole process. We did a total of 6 IUI’s and 2 ICI’s over the course of 10 months. The 2nd through 5th IUI were medicated with clomid, trigger shot, and progesterone suppositories. My 6th, final and sticky IUI was medicated with injectable menopur, trigger, and progesterone suppositories. My 2nd, 4th, and 6th IUIs resulted in BFPs. I lost the first two by 6 weeks. I was very good about taking my supplements for the 2 months prior to starting the injectable cycle and once I started menopur I stopped all supplements, did not do any vigorous exercise, and ate plenty of protein.
Emma2370 – In June ’13 my AMH came back at .39 July ’13 BFP naturally mmc at 8 weeks, November ’13 BFP ended in chemical pregnancy. December.’13 natural BFP healthy baby girl. I took my prenatal and royal jelly supplements. We had no issues getting pregnant staying pregnant with a healthy viable pregnancy was the issue. My DH has an chromosomal inversion which could have contributed to our losses. We did make an appointment with a RE just before our BFP.
2RedTulips – My OB ordered my bloodwork in July 2013, and that’s when my AMH came back at 0.2. I was devastated. We had already suffered one miscarriage and had been trying again for eight months at that point.
With those results, OB sent me to an RE, and we did a full work-up. In addition to my low AMH (tested at 0.8 at the RE’s), DH had poor morph, and we were given a less than 2 percent chance of conceiving naturally. Devastation #2. The one piece of good news I received during that time was that I had 12 resting follicles, which was a big shock.
We both started a slew of supplements per the RE. I also started a low-gluten diet, acupuncture and baby aspirin.
We were gearing up for a first round of IUI (certain we’d have to do IVF after a cycle or two) when I got a BFP. So, I call this baby our “2 percent baby,” because he ducked in under the wire.
So, from the time we received the low AMH results to conception was four months.
ETA: I am 39, by the way. I also took all the supplements with the RE’s blessing (L-Arginine, DHEA (prescription compound only), DHA, Inositol, Vitamin C, Vitamin E, CoQ-10 and Melatonin)
Eliz77 – My AMH was tested twice under two different REs and came back at 0.27 both times-tested in August 2013 and January 2014. Both REs recommended we try naturally for two cycles and if no success, move on to letrozole and IUI. We did get pregnant both times one 2nd cycle, 1st time ended in natural MC at 7 weeks. This one is far from a success story, but doing better than previous.
However, neither RE felt the low AMH was reason for losses or cause of concern. It was explained to me as having a lower egg reserve due to AMA, not necessary an indicator of quality since all other results came back normal.
Due to 2nd RE’s discovery of two copies of the MTHFR c77t gene, I was put on low dose aspirin, folate and started lovenox and calcium once an intrauterine pregnancy was determined. I know opinion vary on whether this is reason alone for losses, but since it was the only thing found amiss, RE decided to be proactive in his treatment plan just in case.
If we lose this pregnancy, my RE has already said he would like to move to IVF with PGD.
Daisy19782011 – Age 35, AMH .16
Did a back to back IUI with injections (gonal F) and a trigger. Got pregnant on 1st cycle. I lost that baby at 19 weeks, unrelated to IF, and did the same protocol 3 months later and got pregannat again. All of my other numbers are OK though, and we have not MFI.
BootsOrHearts –
I am trying to remember my AMH number from way back, I think it was 0.25 I’ll have to ask my doctor as the online records don’t go back that far.
Jan 2012: AMH 0.25 (?) @ 38 years old, diagnosed with DOR, told we are unlikely to get pregnant except via IVF or donor eggs.
Later that month. . . . natural BFP! Loss at 18 weeks, unrelated to DOR diagnosis
Started taking DHEA, one pill/day
2012/early 2013 Lots o’ failed fertility treatments, but good response to IVF, estrogen priming protocol: 7 retrieved, 7 mature, 5 fertilized (with ICSI) and 4 available for transfer, 2 implanted (resulted in C/P) and 2 frozen
April 2013. . . natural BFP @39 years old. Isaac, a.k.a. Baby Boots born 11/23/13.
egsquared –
I had 4 early losses between September 2011-August 2012. In October of 2012, my AMH was .18 at 36 years old. All my other results were normal, and two different RE’s recommended IVF. We had to wait until January 2013 to do an IVF cycle (switched to DH’s insurance). I had 9 eggs retrieved (which I thought was a low number), 5 fertilized with ICSI and two available for a 3 day transfer. we implanted both and got pregnant that cycle. DS was born 4 weeks early in September 2013.
In the months leading up to our IVF cycle, I took DHEA, CoQ10 and myoinositol.
The RE explained that with low AMH, you have a higher percentage of abnormal eggs left, so I was probably having bad luck and getting BFP’s on the cycles where my body released a bad egg. He said we could just keep trying naturally and we could get lucky and get a ‘good’ egg and a BFP, whereas with IVF we would be picking the best looking embryo(s) out of the group. We chose to go the IVF route to hopefully avoid any additional losses and because age/time was not on my side.
rslh10 – 28 years old, DX of .58 AMH in March 2014. Started Clomid CD 3-7 with trigger on CD 15, BFP the first try, but ended up ectopic @ 5w6d.
I was taking prenate minis, vitamin D, and biotin. Also my FSH was 7.5, and all the other blood work that had been drawn has been normal. HTH